The Illness That Never Really Leaves
We’ve all had a stomach bug the kind that floors you for a day or two, followed by days of bland food and cautious recovery. But what happens when that temporary illness leaves behind a lasting change in your gut? For many, the infection fades, but symptoms like bloating, urgency, and irregular bowels stick around for months or even years.
This isn’t in your head. It’s a medically recognized condition known as post-infectious irritable bowel syndrome (PI-IBS), and it’s far more common than most people and even some doctors realize.
What Is Post-Infectious IBS?

Post-infectious IBS is a subset of irritable bowel syndrome that develops after an episode of acute gastroenteritis commonly caused by food poisoning, bacterial or viral infection, or contaminated water. Unlike traditional IBS, which has multifactorial roots, PI-IBS has a clear starting point: an identifiable infection that seems to flip a permanent switch in gut behavior.
Even after the infection clears, the gastrointestinal system doesn’t go back to baseline. Patients report altered bowel habits, abdominal discomfort, gas, and food sensitivities they never had before. These symptoms persist long after pathogens are gone, making it both a frustrating and confusing condition.
How Does It Happen?
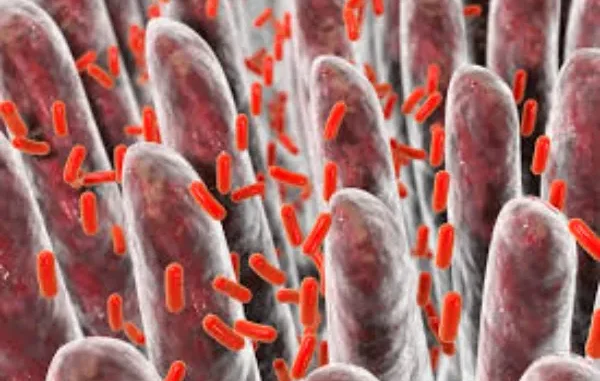
During an acute infection, the gut lining becomes inflamed as part of the immune response. For some individuals, this inflammation doesn’t fully resolve. Instead, it leaves behind a state of low-grade inflammation, altered gut motility, and changes in how the body perceives gut signals known as visceral hypersensitivity.
The gut microbiome also takes a hit. Beneficial bacteria may be depleted, while harmful strains can flourish. This dysbiosis can further interfere with digestion, increase gas production, and exacerbate immune responses. The result? A gut that reacts differently to the same foods and routines that once felt normal.
How Common Is It?
You’re not alone. Studies suggest that 10-30% of people who experience an episode of gastroenteritis go on to develop PI-IBS. The risk is higher if the infection was severe or prolonged, involved vomiting and diarrhea, or if antibiotics were used.
Other risk factors include female gender, pre-existing anxiety, and stress during or shortly after the infection. While anyone can develop PI-IBS, these factors increase the odds.
Whether you’re consulting a local physician or a gastroenterologist in India, this specific subtype of IBS is increasingly being recognized and studied and that’s a good thing, because awareness is key to targeted care.
Symptoms to Watch For
PI-IBS symptoms closely mimic classic IBS, but with the added context of starting soon after a stomach infection. Common complaints include:
- Persistent bloating and gas
- Diarrhea, constipation, or alternating patterns
- Abdominal cramping, especially after meals
- Urgency to pass stool
- Food intolerances that didn’t exist before
- A feeling of incomplete evacuation
What makes PI-IBS tricky is that standard tests like endoscopies, scans, and blood work often return normal. That’s because PI-IBS is a functional disorder where the gut’s function is impaired, but not visibly damaged.
Diagnosis: A Process of Elimination
There is no single diagnostic test for post-infectious IBS. Diagnosis is usually clinical based on symptom patterns and history of a prior infection. Your doctor may rule out other conditions like inflammatory bowel disease (IBD), celiac disease, parasites, and bile acid malabsorption before arriving at PI-IBS.
A thoughtful consultation and detailed symptom history are essential. Sometimes stool tests, blood work, and imaging are done not to diagnose PI-IBS, but to exclude more serious conditions.
With the rise of health technology like microbiome analysis kits, remote symptom tracking apps, and AI-assisted assessments, healthcare is becoming more tailored to the individual. These technological shifts are transforming how chronic gut conditions are monitored and managed especially in cases where traditional testing falls short and ongoing data insights offer more targeted solutions.
How It’s Treated
The good news is that PI-IBS can be managed and in many cases, improved significantly. Treatment generally focuses on symptom relief, microbiome restoration, and reducing gut hypersensitivity.
Dietary Management
Many patients benefit from a low FODMAP diet, which reduces fermentable sugars that fuel gas-producing bacteria. However, this diet should be followed under professional guidance, as long-term restriction may harm the microbiome.
Probiotics and Prebiotics
Targeted probiotics may help rebalance gut bacteria, though not all strains are effective. Prebiotic fibers can also support recovery but should be introduced cautiously.
Gut-Directed Therapies
Medications like antispasmodics, gut-specific antibiotics (e.g., rifaximin), or bile acid binders may help depending on symptoms. Neuromodulators like low-dose tricyclic antidepressants are often used not for mood but to calm gut nerve sensitivity.
Lifestyle and Stress Reduction
Stress is a known trigger for symptom flares. Techniques such as gut-directed hypnotherapy, CBT, yoga, and breathwork have shown real benefits in reducing flare-ups and improving quality of life.
How Long Does It Last?
Recovery from PI-IBS varies widely. Some people return to normal within months, while others deal with symptoms for years. Early intervention tends to improve outcomes. Over time, many patients experience fewer flares, better food tolerance, and a return to regular digestion especially when diet, stress, and microbiome health are all addressed together.
The goal is to reduce symptom burden and improve quality of life not just manage flare-ups. And thankfully, that’s becoming more achievable with today’s integrative and personalized approaches to care.
When to Seek Help
If your gut hasn’t felt the same since a bout of food poisoning, traveler’s diarrhea, or gastroenteritis, don’t ignore it. Chronic digestive symptoms are not just something to “get used to.” Working with a trained provider can uncover not only the root cause but also practical ways to reduce symptoms without unnecessarily restricting your life.
If you’ve already ruled out conditions like IBD and celiac disease but still struggle, ask your provider if post-infectious IBS could be the cause. Nowadays seeking help from a doctor does not take that much time due to online doctor consultation services.
A Condition That Deserves Attention
PI-IBS is a clear example of how even a short-lived infection can lead to long-term digestive consequences. It’s not just “all in your head.” It’s a biologically driven, microbiome-disrupting, gut-altering reality that deserves more awareness and better care.
The silver lining? With the right guidance, patients can experience real relief. Through strategic dietary changes, microbiome repair, and stress modulation, the gut can be brought back into balance. The key is knowing what you’re dealing with and not settling for vague labels when answers exist.





Leave a Reply